By: Jonathan Ahmadi
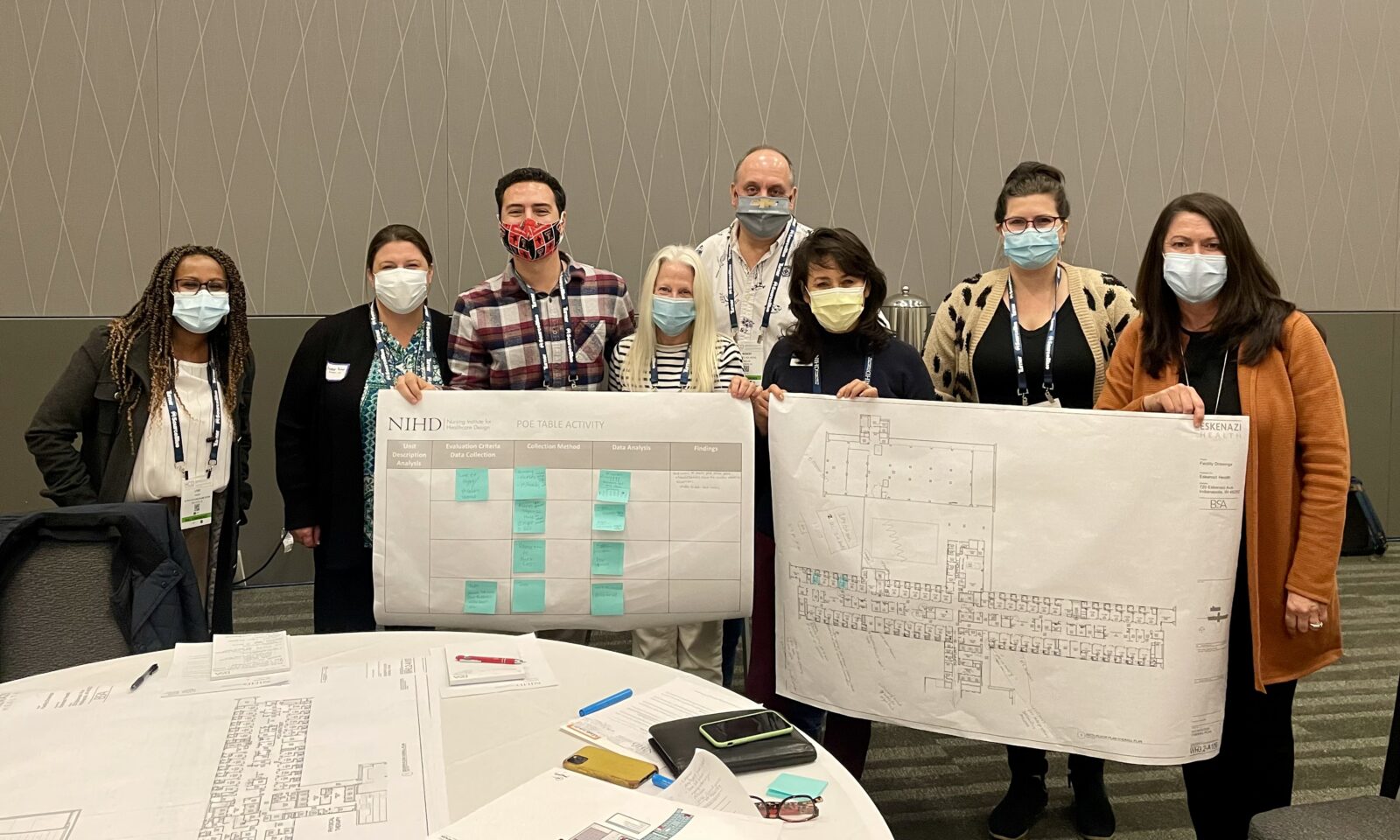
Yellow Brick is proud to share that our President and CEO, Kelly Guzman, will serve as the 2022 President of the Nursing Institute of Healthcare Design (NIHD). The Nursing Institute of Healthcare Design is a national organization that focuses on sharing clinical expertise to influence the planning and design of built healthcare environments. NIHD’s vision is to advance clinicians’ involvement at the forefront of the design development process to ensure healthcare spaces support clinical care and the staff who work within those spaces.
Kelly’s experience leading Transition and Activation Planning projects will be invaluable in her role. When working with end-users to validate workflow and operations in the new space, Kelly and her team help translate the functional narrative of project design. She looks forward to sharing her experience and collaborating with others to further the clinical role in design planning.
Kelly was first introduced to NIHD by Debbie Gregory, one of the cofounders of NIHD. Kelly has been active in many organizations throughout her career, including the Emergency Nurses Association, the Association of California Nurse Leaders, and the National Association of Hispanic Nurses. Despite providing great value, none of these organizations focus on healthcare design or Transition and Activation Planning. When she learned about NIHD, Kelly knew she had to be involved. In her words, “NIHD is an organization of people with a common goal of taking their clinical expertise and applying it to the built environment.”
Yellow Brick Project Manager, Jonathan Ahmadi, sat down with Kelly to discuss her new role, goals for the year, and why the clinician’s role in the design process is vital to healthcare construction.
Can you share some examples of how design decisions have downstream impacts on clinical teams, operations, and workflow?
A great example of the impacts design decisions can have on teams’ day-to-day operations is decentralized patient care or nursing stations. Patient care stations are key elements of the clinical environment. You do a lot of teaching and collaboration there, get clinical advice, and discuss case studies and problem-solving that you can apply to your practice.
In the old days, each department had one nursing station, so when planning to activate a new environment, the clinician’s mindset centered around working in one central location. Decentralized stations require an entire mind shift. A key challenge is figuring out how to work with staff to accept the space and manage the stress of how their world will change. When we are working with teams, the worry is that you’re going to lose some of the collaboration and teamwork, so it’s our job as the transition team to provide solutions and recommendations.
Our team has observed that clinical teams are able to embrace the change and ultimately feel like the new design is better for the patient and them. Teams must adapt their workflows, use technology to communicate, embrace growing pains, and learn how to collaborate and teach in this new environment to get this point.
The period from the design phase to when people are working in their new space can be long, sometimes even more than ten years. I imagine most designers don’t get the opportunity to reevaluate and understand what worked and what didn’t work. As NIHD President, I see you being able to provide a lot of value in bridging that gap, having worked through the full project lifecycle on multiple projects.
Yes, and interestingly, at the 2021 Healthcare Design Conference, our focus was on the post-occupancy evaluation. We included representatives from all phases of the project and got to hear each person’s perspective. This continues to be a focus for us at NIHD, bringing together interdisciplinary teams to share lessons learned. From a post-occupancy perspective, we must understand the support systems and the resources available to each organization. One organization may have strong working relationships between the physicians, nurses, and ancillary teams, enabling them to implement new design initiatives successfully. Those same design initiatives may not work at another organization that does not have those same relationships established. Alternatively, positions and resources at a larger academic medical center may not be available in a community hospital. When considering these lessons learned, ensure you’re comparing apples-to-apples and that the organization has the resources required to implement the suggested approach.

You’ve taken on this role because you think your experience will help to bring value to the organization, but I’d love to hear from you in what ways you think your time with NIHD has made you a better project manager and a better transition planner.
The opportunity to collaborate with people who have been through similar experiences has been advantageous. There is a spirit of collaboration and information-sharing, even working with some of our competitors. We have a member forum where you can share information and ask questions. We take those conversations, webinars, and conferences, and archive them for future use. So, for example, if I have a project on behavioral health, I’m able to go back and access the resources of those lessons learned that we’ve shared. The collaboration and expertise of the NIHD members and the ability to collaborate when I have questions have been highly beneficial.
In what ways do you feel volunteerism enriches your own life?
I spent the first twelve years of my nursing career at a faith-based organization where there was a lot of giving back to the community. I have been fortunate to have been the recipient of scholarships to help me with my education. When I was starting out in my career, I was lucky to have people in organizations who allowed me to trial some of the leadership practices I learned. I have been mentored by people who took the time to answer my questions and help me grow. I think it’s essential to take the wisdom and blessings you have received in your life and share them with other people. It’s part of my DNA.
Could you give us a peek into the future? What are some of the significant changes you anticipate coming in healthcare design?
As a result of the pandemic, we have had to quickly embrace telemedicine or healthcare that isn’t necessarily in a clinic or a hospital setting. I believe we are at the cusp of something very new, and I find this intriguing. We can now receive care outside of hospitals or the doctor’s office. In the future, I would say that there will be a hybrid approach to medicine and changes to how we administer care. There is a more significant focus on the total wellness of clinical teams. Healthcare providers especially have been stretched during the pandemic. It isn’t just the physical effort but also mental well-being. Buildings designed to support respite and amenities that bring joy to staff and patients will be trends I foresee in the coming years.