By: Kelly Guzman
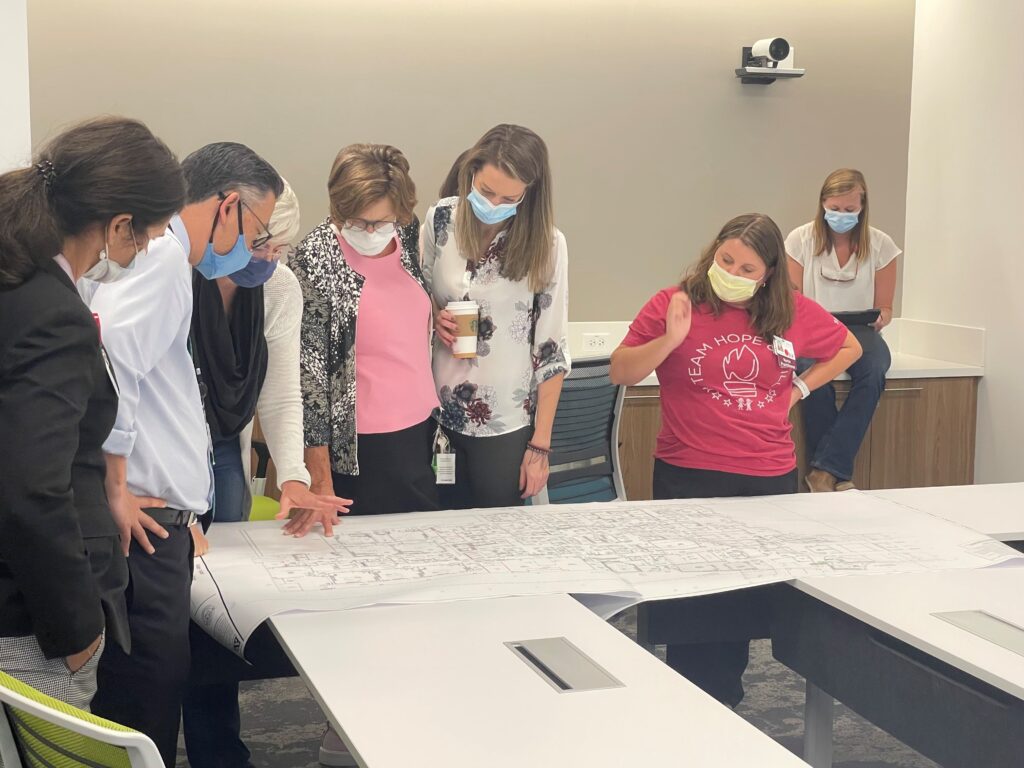
The design phase of a healthcare project typically includes the project team (architects, engineers, planners, etc.) and the owner, with representatives from the organization responsible for providing input on the facility’s layout and requirements (typically administration and directors). Identifying a small cadre of frontline staff to provide input on design can increase project engagement and provide insight into the operational workflow. Most healthcare representatives are unfamiliar with new facility planning or design. Additionally, they may not have the expertise needed or be accustomed to the architectural jargon used to communicate with the project team. The organization’s healthcare team relies on the architects to serve as the experts and represent their needs, while the architects rely on the healthcare team to provide operational input and respond accurately to their requests.
Over the past 15 years, our team has assisted in activating over 70 new healthcare facilities across North America. As a result of our experience, we have identified common operational and regulatory issues that often arise during the activation phase. Bridging the gap between design and activation, we expanded our services to include Design Strategy Consultation, in which we partner with organizations to share our expertise during the design phase to prevent these common issues in the activation phase.
This article shares some of the most common issues we encounter when activating a new healthcare facility. Our goal in sharing lessons learned is to provide education to avoid these issues and mitigate costly operational and regulatory challenges during activation.
Eyewash Stations
Eyewash stations are required based on Occupational Safety and Health Administration (OSHA) guidelines and in accordance with the organization’s policy. Ensure your organization’s policy and practice are consistent. Requirements for emergency eyewashes and showers are cited in OSHA 29 CFR 1910.151(c): “Where the eyes or body of any person may be exposed to injurious corrosive materials, suitable facilities for quick drenching or flushing of the eyes and body shall be provided within the work area for immediate emergency use.” OSHA refers employers to the American National Standards Institute (ANSI) Z358.1-2014 https://webstore.ansi.org/Search/Find?in=1&st=Z358.1-2014 for additional guidance on protecting employees exposed to injurious corrosive materials. One topic that often becomes a point of discussion is the ANSI standard for an eyewash station to be in an accessible location no more than 10 seconds walking time from a hazard location. The eyewash location must be on the same level as the hazard (no stairs or ramps), and the path of travel must be free of obstructions (no doors) that may inhibit its immediate use. The eyewash station should also be located in an area identified with a highly visible sign positioned so the sign shall be visible within the area served by the eyewash.
Recommendation: The planned locations of eyewash stations can become problematic when there is a change of service in the space. Change is inevitable, so if your organization is moving service lines and patient populations, best practice includes a review of the types of materials and chemicals stored and required to care for the patient population to confirm if an eyewash station is required.
Infection Prevention and Control
The planned locations of wall-mounted items, such as dispensers for alcohol-based hand rub, soap, paper towels, and holders for sanitizing wipes and personal protective equipment (PPE), often do not support operations or infection prevention and control standards. It is prudent to check the quantity of alcohol-based rub in rooms, corridors, and storage rooms to ensure they comply with NFPA and other regulatory limits.
Element(s) of Performance for LS.05.01.30 effective July 2021
Alcohol-based hand rubs (ABHR) are stored and handled in accordance with NFPA 101-2012:8.7.3.1 as follows:
- Corridor clear width of 44 inches is not compromised by the dispenser
- ABHR does not exceed 95% alcohol
- Maximum individual dispenser capacity is 0.32 gallons of fluid (0.53 gallons in suites or rooms separated from corridors) or 18 ounces of NFPA Level 1–classified aerosols
- Dispensers have a minimum of four feet of horizontal spacing between them
- Dispensers are not installed within one inch of an ignition source
- If the floor is carpeted, the building is fully sprinkler protected
- Operation of the dispensers must comply with the manufacturers’ instructions for use
- ABHR is protected against inappropriate access
- Not more than an aggregate of 10 gallons of fluid or 135 ounces of aerosol is used in a single smoke compartment outside a storage cabinet, excluding one individual dispenser per room
- Storing more than five gallons of fluid in a single smoke compartment complies with NFPA 30
We have found that ADA regulations may require a less than optimal placement of some of these items. An example that we frequently observe is that due to space limitations, paper towel dispensers may need to be installed on an adjacent wall rather than immediately adjacent to the sink to be in compliance with ADA dispenser height placement regulations. As a result, this can result in a slip hazard as water may drip on the floor due to the distance between the sink and the paper towel dispenser.
Recommendation: We recommend that organizations create mock-up rooms to validate the placement of wall-mounted items prior to beginning installation. This can be done judiciously by using props to create a room in order to be fiscally conservative. Develop a checklist with the required room contents and confirm the placement in each room type. If rooms are not standard sizes or layouts, establish guidelines with team preferences for adjacencies and installation of items that need to be next to each other. We recommend including frontline staff, an Infection Preventionist, an ADA specialist, and a regulatory expert to confirm compliance with regulatory requirements and validate the various items’ height and location requirements.
Regulatory Required Signage
We have learned that the required regulatory signage (EMTALA, patient rights, etc.) is not typically included as part of the facility signage package. Although signage can be ordered, the challenge often lies in identifying wall space and backing needs for these required postings.
Recommendation: Include a member of the organization’s regulatory team who is familiar or an expert with regulatory signage during design to confirm locations and space are confirmed.
Doors and Access
The most common issues in a new facility are related to the type of door hardware selected and access to spaces. Soiled utility rooms are required to be locked due to hazardous contents being stored in the room. If staff brings contaminated materials to the room, it is ideal to install badge readers to control access and to reduce the risk of a spill or accident occurring while staff’s hands are full of soiled items. In operating rooms and other sterile spaces, the use of wave plate technology on doors is excellent for hands-free access. Sensors will need to be strategically located to prevent doors from inadvertently opening when someone passes by. It is helpful to have an override to turn off the wave plate sensor once the team is in the room to prevent this issue. If there are contiguous wave plates it is recommended that signage be added to clearly identify which plate opens which area.
We recommend that cabinetry have a consistent lock core and key. One key promotes compliance with requirements for locked items and increases staff efficiency by minimizing the number of keys required per department. It sounds intuitive, but we have been in many facilities where this issue has been identified during Dress Rehearsal, resulting in a locksmith having to replace many lock cores on brand-new cabinets to enable the use of a single key.
Recommendation: Establish an interdisciplinary workflow team to review the planned door hardware and access throughout the new facility. Include department representatives, as well as team members who will access various spaces throughout the facility, including security, facilities, environmental services, infection prevention and control, and code responders. Tabletop Exercise is another method to validate access, as it provides staff the opportunity to talk through a scenario using floorplans.
Ligature Risk
We have recently noted an increase in spaces designated for behavioral health patients. Ligature-resistant furniture, fixtures, and equipment should be planned for these spaces. Most of the rooms have minimal storage and have locked cabinetry with tamper-resistant finishes.
Recommendation: Convene a team familiar with the patient population, treatment protocols, and equipment and supplies required in or near the room to conduct a risk assessment of the space. The team should also include representatives from the department, medical staff, facilities, security, regulatory, environmental health and safety, psychiatry specialist (if available), and infection prevention and control. A best practice is to have the team sign off each room using a checklist.
Staffing Support of Daily Operations
This one is always tricky and often is very specific to each organization’s situation. A regulatory body can approve the design because it includes staff support to bridge a gap in the physical requirements. An example is the use of 1:1 staffing with sub-nursing stations to support the line of sight to the patient. Space can be approved with this model, so if there are changes in the staff support, there could be an issue with regulatory sign-off. Other staffing impacts may result in regulatory gaps if there are assumptions regarding staffing to support specific spaces such as observation areas. If the staff is removed, there may be licensing issues if there is no staff to provide observation or the role required for compliance.
Recommendation: To avoid this issue, we recommend using a Decisions Document to track all decisions that need staff or operational support for regulatory compliance. If possible, engage with local regulatory agencies early to review the area’s decisions and assumptions to gain buy-in for the staffing support plan. If the regulatory agency is amenable, include them in an early tour of the new facility with Blueprints to help identify early concerns.
Preparing for Survey
We recommend that the organization conduct an early assessment from a regulatory perspective to identify facility issues that require modification during the activation phase. Start preparing for the state regulatory survey and any other required inspections early and continue to refine the plan throughout the project’s lifecycle. It is best to not assume the existing facility methods are compliant with regulatory requirements. Confirm and verify that all new features, systems, rooms, spaces, etc., are compliant with current requirements. Incorporate regulatory compliance and infection prevention and control review into all facility planning activities, including design review, furniture and finish selections, and designating paths of travel. Consider the development of scripted survey responses to support transparent, concise, and consistent staff answers to common surveyor questions. Incorporate scheduled mock surveys into the preparation process to instill confidence in the staff to safely perform their jobs in the new facility.
We wish you the best on your activation journey.

