By: Kelly Guzman
“What do you do?”
This is the most common question I am asked by people whom I am meeting for the first time. My typical response is, “I’m a healthcare project manager who works with organizations to activate their new buildings.” Sometimes this helps, but people often respond with, “so what does that mean?” To further clarify, I reply, “I’m like a wedding planner for new healthcare facilities.” Bingo! The light bulb goes off.
Transition and Activation Planning in healthcare has evolved over the past decade. When I began my career as the Director of Transition Planning at UCLA in 2004, there wasn’t a clear understanding or definition of Transition and Activation Planning. During my 15-year career as a Transition and Activation Planning consultant, my team and I have developed a streamlined and effective process that healthcare leaders can leverage on their new facility projects. At Yellow Brick, we define Transition and Activation Planning as the process of planning and implementing the opening of a new healthcare building or space. As a Transition and Activation Planner, my job is to help clients prepare for and coordinate all aspects of the activation, much like a wedding planner does for the couple’s big day.
Our work as Transition and Activation Planning project managers involves applying the design concepts from the Functional Narrative or Basis of Design documents provided by the architect to the built environment. Typically, there is a lag of three or more years from design development to construction completion on healthcare projects. As a result of this lag, new people who did not participate in the design, lapse of memory of decisions, regulatory changes requiring adjustments, and inflation can all impact the project’s overall success. These pain points often reveal themselves during the Transition Phase, as organizations are focused on developing new operational plans, including staffing plans, budgets, workflows, equipment and technology integration, and functional adjacencies that will impact their new world. Transition activities add up to a lot of change.
In my experience, people like the idea of change, but not the process. Therefore, organizations must identify Change Champions to successfully drive the change to transition. The transition period is when the clinician’s perspective and experience is crucial. Clinicians spend their days prioritizing and reprioritizing their workload as new patients are admitted, patient status changes, new orders are entered, systems go down, equipment doesn’t work, etc. To do this, they must have a comprehensive understanding of their work and the inputs from other departments and systems. This experience is invaluable to the planning of a new facility. The clinicians best understand bottlenecks and support systems needed for efficient operations. They are well-positioned to represent the organization in its needs.
Clinicians are trained using an ADPIE framework that translates well with Transition and Activation planning. ADPIE is Assessment, Diagnosis, Planning, Implementation, and Evaluation. When approaching the unknowns of a new facility project, this model promotes prioritizing the most critical work.
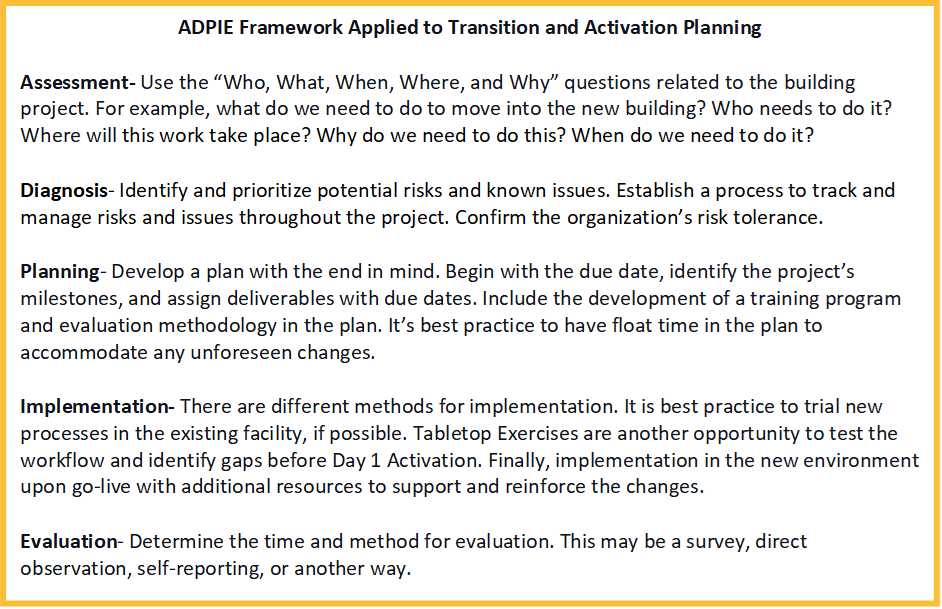
The clinical perspective and influence in the organization will help communicate the change messages, translate the work that needs to be completed and prioritize this for the team. There are hundreds of new workflows that need to be reviewed, re-engineered, and implemented. The approach is scalable and can be used to develop a plan for the project (the entire new building), for a department (e.g., Emergency Department), or a workstream (e.g., patient transport.) Clinicians can help determine which workflows and systems are most critical to operations and must be completed before moving into or activating the new space.
Due to the increasingly complex nature of healthcare facility projects, clinical representatives are required members of an integrated project team. Their participation is invaluable in translating the frontline staff’s needs to the project team, prioritizing clinical needs versus wants, and serving as change agents to implement the new processes. As you begin to plan for your next Transition and Activation project, ensure you engage your clinical leaders. Their perspective and insight will be critical drivers of adopting organizational change and project success.

