By: Christina Olivarria
When building a new healthcare facility, the major change focus of the organization is typically on the physical change that will occur as a result of the construction of the new environment. The construction of this new space results in massive changes for the organization, including location, workflow, technology, equipment, and systems. These changes are generally managed by either the internal departments impacted by the change or by contractors that specialize in the specific components of the project. What organizations often fail to account for is the people and operational impacts that will occur. It is imperative for the organization to incorporate these elements into the planning. The Prosci® ADKAR® Model is a process that can be used in combination with Business Relationship Management to plan for the transition and activation of a new space. Failure to effectively plan can lead to resistance from organizational stakeholders to adopt the new workflows, technologies, and systems, thus creating a disconnect between intended design and actual usage.
Transition and Activation Planning is the process of planning, implementing, and evaluating the physical (Building Readiness) and human (People Readiness) components that support the opening of a new space or building. The project management goal is to transition the organization’s current operations to an optimal future state in the new building, creating a fully functional facility. Transition and Activation Planning activities occur in the following phases:
- Project Start-up- During this phase, the Transition and Activation Project Manager will build the project plan, incorporating the basis of design and intended value elements. Outputs include governance structure, stakeholder identification, project schedule, budget, work breakdown structure, risk management plan, and communication plan.
- Transition and Occupancy Planning- During this phase, the Transition and Activation Project Manager will engage organizational stakeholders in the operational planning of the new space. This includes the creation of new workflows, policy and procedure review, orientation and training plan and workforce analysis.
- Activation Planning- During this phase, the Transition and Activation Project Manager will work in conjunction with the organizational departments to make ready the space. This includes the facilitation of new facility and department-specific orientations, interdisciplinary simulation exercises, issues management, and the move into the new space.
- Stabilization- During this phase, the Transition and Activation Project Manager will work with organizational leadership to prioritize, manage, and resolve issues. In addition, the team will continue to conduct orientations and refresher training for stakeholders. Performance metrics will begin to collect data, and processes will be adjusted to meet operational needs.
The Prosci® ADKAR® Model is a goal-oriented change management model that focuses on the two dimensions of change: business and people. In conjunction with Transition and Activation Planning, the ADKAR model can be used by healthcare organizations to better anticipate the impacts of change, and thus proactively plan. Looking closer at the change management lifecycle of a new healthcare facility, the illustration below depicts how the two processes can be blended to allow healthcare organizations to successfully achieve intended the goals and value of a new facility.
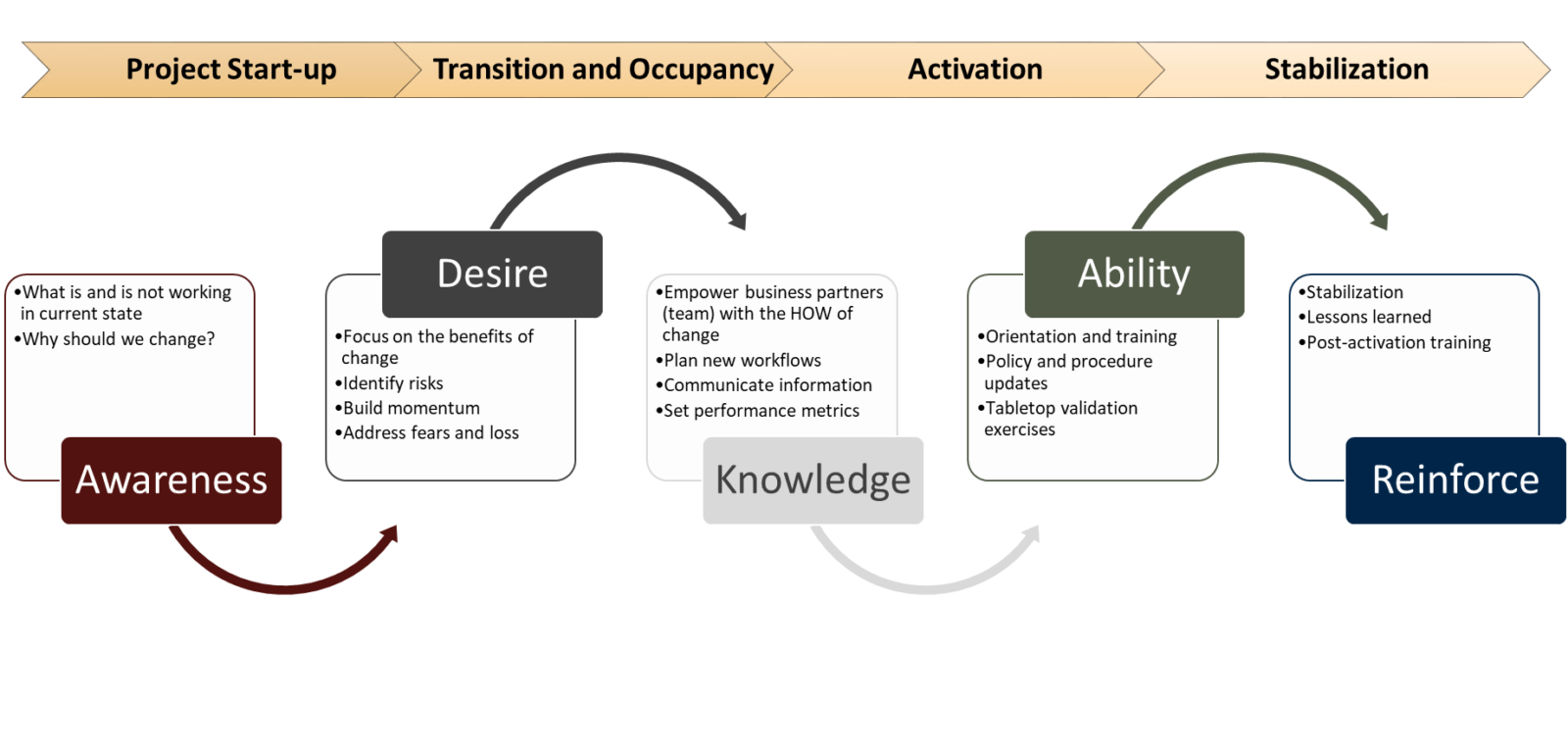
During the project start-up phase of the Transition and Activation project, the project manager can tackle the first phase of the ADKAR. This phase combines both the business and people side of change. It revolves around understanding the need for change and the goal is to define the clinical and operational outcomes that the project intends to deliver. It is important for the organization to engage frontline stakeholders during this phase of the project, as they can provide a unique insight into the current state of the organization: what is working and what can be improved. This insight can then be included in the programming aspects of technology, systems, equipment, and project guiding principles. One of the key questions that should be answered during this phase of the project is the ‘why’ of change. Why is the organization building this new space? Why do processes need to be updated? Why should I, a frontline stakeholder, rally behind this change? Answering these questions will feed into the next step of the ADKAR model: desire.
In order to create a desire for change, the Transition and Activation Project Manager first needs to understand the culture and organization’s maturity. This will allow the project manager to create a plan that uniquely addresses both the needs and the capabilities of the organization. Culture has the ability to both advance strategy and to destroy it, so taking the time to evaluate the type of culture that exists in the organization will strengthen the project manager’s execution of strategy. Additionally, understanding the capabilities of the organization is equally as important when addressing the subject of desire. Whether it be through the utilization of Capability Maturity Model Integration or Organizational Project Management, the assessment of maturity can reveal the organization’s readiness and capability, expressed through its people, processes, data, technologies, and the consistent measurement practices in place.
Once both culture and maturity are understood, the Transition and Activation Planning Project Manager can foster that desire to change in impacted stakeholders through the activities of the transition and occupancy planning phase. This includes addressing the benefits and risks of change, addressing the fears of change and the sense of loss that stakeholders may communicate, and then building a work breakdown structure that incorporates these elements into the strategy. Including stakeholders, especially those that will occupy the new space, will employ a greater sense of buy-in and reduce the resistance to the adoption of change.
Prior to moving into the knowledge component of change, it is imperative to note that without addressing both the awareness and desire components, a change management strategy will be disadvantaged. Engaging stakeholders in the operational planning and overall orientation plan will allow a program to be designed that addresses the unique needs of each department. This component will take place through both the transition and activation phases of the project. Communication will play an important role during this phase, especially as decisions are made and activities begin to ramp up. Using methods such as town halls, dashboards, visualization boards, intranet, and team huddles, will aid in the dissemination of these decisions and provide stakeholders the ‘how’ of change.
During the activation phase, the building will be turned over to the owner to begin preparing for Day 1 Operations. As the space is being fit-up with new furniture, fixtures, and equipment, training can simultaneously be conducted. All frontline staff that will either work in or supports the new space will require new facility orientation to new building components. Additionally, policies and procedures will need to be updated to ensure that they align with the decisions made during the transition phase. Prior to patients occupying the new space, it is recommended that validation exercises take place to confirm that the planned operations and workflows are functional and to ensure that any issues identified have been mitigated. These activities ensure that stakeholders are confident in their ability to perform their roles in the new space.
Once the building is open, the organization enters the final phase of the Transition and Activation Planning project: the stabilization phase. During this phase, the organization will reinforce the change through the evaluation of processes and performance metrics. These metrics will determine if the organization achieved the clinical and operational outcomes that were originally intended. An important lesson learned during this phase is the recognition that issues identified during the previous phases may still exist, so issues management practices will still need to be in place. Staff may require refresher training on new systems, technology, or equipment, so ensure that there are resources available to reinforce the planned functions of the new space. This will smooth the project from the transition to daily operations.
The role of the Transition and Activation Project Manager throughout the lifecycle of the project is vital to the project’s success. Whether this role is filled by an internal resource or a contractor, the designated individual should serve as the Business Relationship Manager for the organization and is responsible for project strategy, implementation, and realized value. Working as a liaison between organizational leadership and end-users, this individual works to create processes that align with organizational needs and also communicate the vision to teams, thus optimizing value. Working as a trusted advisor, the Transition and Activation Project Manager should not only assess the current state of the organization but should also work to improve capabilities by creating best practices and standard processes.
“The rate of change is not going to slow down anytime soon. If anything, competition in most industries will probably speed up even more in the next few decades.” – John P. Kotter
Recognizing both the business side and people side of change during the activation of a new healthcare facility is critical to project success. Applying the ADKAR model to the Transition and Activation Planning methodology will ensure that the people side of change is not just an afterthought, but is woven into the project plan, maximizing business value and stakeholder buy-in. As a Business Relationship Manager, the Transition and Activation Project Manager can work alongside organizational leadership to design processes and plans that are sustainable and achievable, thus optimizing patient care and organizational practices.

